- News
A Ray of Hope in Total Darkness: Vision Saved 48 Hours After Retinal Artery Occlusion | A Breakthrough Eye Surgery at Shanghai General Hospital
Total blindness in one eye, and now sudden complete vision loss in the other — with the golden treatment window already missed. Can vision still be saved?
For 45-year-old Mr. Qi (pseudonym), life had long been overshadowed by illness. Years of diabetes had led to severe retinal complications, and his right eye was already permanently blind due to neovascular glaucoma. His left eye — after undergoing vitrectomy, cataract surgery, and panretinal photocoagulation — retained just enough vision to keep him connected to the world.
But suddenly, disaster struck: his only seeing eye went completely dark.
It wasn’t until 48 hours later that Mr. Qi was transferred to Shanghai General Hospital, home to the National Clinical Research Center for Ocular Diseases. The diagnosis was grim: central retinal artery occlusion (CRAO) in the left eye.
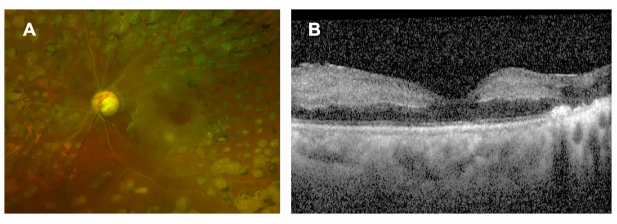
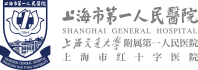
Figure 1: Retinal artery whitening (A); intracellular edema at the macula (B)
CRAO: A Stroke in the Eye With No Way Out?
Central retinal artery occlusion — often referred to as an “eye stroke” — is one of the most vision-threatening emergencies in ophthalmology. After just 90 minutes of ischemia, retinal neurons begin to die irreversibly. Beyond 4 to 6 hours, the chances of saving vision become vanishingly small. By the time Mr. Qi arrived, 48 hours had passed.
His case was further complicated by:
Monocular vision: Right eye blind; left eye was the last hope.
Missed golden window: Far beyond the critical 6-hour period.
Poor general health: End-stage renal failure due to diabetes, requiring dialysis every other day.
Complex surgical history: Previous vitrectomy limited options like ocular massage and anterior chamber paracentesis.
Faced with what appeared to be an irreversible fate, the team — Dr. Liu Haiyun, Dr. Sang Yanzhi, and Dr. Wu Yidong — made a bold decision: to fight for the last glimmer of light.
Breaking the Deadlock: Micron-Level Intra-Arterial Thrombolysis
To treat this seemingly hopeless case, the ophthalmology team deployed a cutting-edge international technique: retinal arterial catheter-based thrombolysis — one of the few options available for late-stage or otherwise untreatable CRAO cases.
The technique hinges on precision and direct drug delivery. Under a surgical microscope, a 48-gauge micro-needle (only 50 microns in outer diameter, thinner than a human hair) is inserted through the vitreous cavity directly into the central retinal artery. A thrombolytic agent (tPA) is then carefully injected to dissolve the clot, restore blood flow, and salvage dying retinal neurons — all while avoiding the bleeding risks of systemic thrombolysis.
“The challenge lies in the artery’s extreme delicacy,” explained lead surgeon Dr. Liu Haiyun. “It requires extraordinary tactile sensitivity and ultra-steady hands. Meanwhile, the support from our anesthesia and imaging teams is absolutely vital for success.”
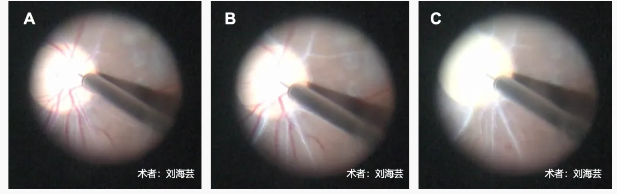
Figure 2: Retinal arterial catheter-based thrombolysis in action.
A Miracle Unfolds: From Blindness to 0.4 Vision
Within one week of surgery, Mr. Qi could count fingers — a sliver of light had returned.
By the one-month follow-up, his corrected visual acuity had miraculously recovered to 0.4 — enough to read large print, recognize faces, and live independently.
Figure 3: Fluorescein angiography showing arterial filling before (limited to inferior nasal branches) and after (full retinal perfusion at 20 seconds). Photo by Dr. Cai Zhengyuan.
“I thought my world had ended,” Mr. Qi said, tearfully. “But the doctors at Shanghai General turned the lights back on. For someone with only one eye left, that 0.4 vision means everything.”
Hope for Others: Who Can Benefit From This Technique?
Retinal arterial catheter-based thrombolysis represents a frontline innovation in treating retinal vascular occlusions. As a national clinical center, the ophthalmology team at Shanghai General Hospital is among the few in China capable of performing this intricate procedure, offering a last-resort pathway to vision for patients once deemed untreatable.
Ideal candidates include:
Patients who have missed the 6–12 hour treatment window.
Those with contraindications to systemic thrombolysis (e.g., active bleeding, recent surgery, poorly controlled hypertension, or coagulation disorders).
Patients unresponsive to conventional emergency treatments (e.g., medications, IOP-lowering, oxygen therapy).
“This is not a miracle cure,” cautioned Prof. Sun Xiaodong, Director of the Ophthalmology Center, “but for selected patients — especially those in critical condition like Mr. Qi — it offers a rare second chance at sight.”
Original by Liu Haiyun, Department of Ophthalmology, Shanghai General Hospital