- News
Media Spotlight | Wenhui Daily: “Panda Blood” Patient with Seven Leg Fractures Saved from Amputation by Multidisciplinary Team at Shanghai General Hospital
https://mp.weixin.qq.com/s/3Lo1QoG6veEOdrsAkqgMkg
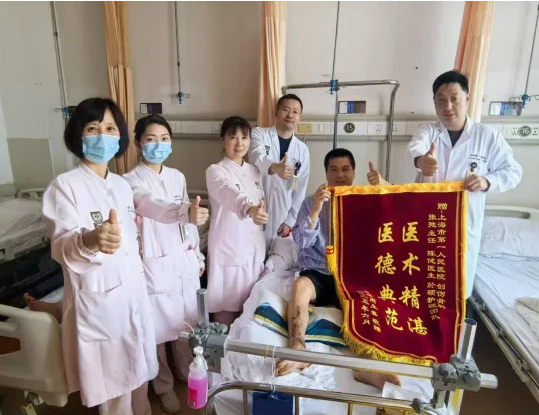
A recent case at Shanghai General Hospital has drawn wide media attention after a multidisciplinary medical team successfully performed a high-risk limb-saving operation on a patient with multiple severe leg fractures and a rare blood type—Rh-negative, commonly known as “panda blood.”Over the course of more than two weeks, the team overcame major challenges including high amputation risk, complex fractures, critical blood shortages, infection risks, and a complicated postoperative recovery. The patient made a strong recovery and was discharged on June 24.
Life-Threatening Trauma Meets a Rare Blood Type
On the night of May 30, a 45-year-old male was rushed to the emergency room of the Hongkou Campus of Shanghai General Hospital. According to Dr. Chen Jian from the Orthopedic Trauma Department, who was on duty at the time, the patient arrived unconscious with a blood pressure of 70/40 mmHg, heart rate of 180 bpm, and hemoglobin level at only 60 g/L. Despite heavy dressings, both heels were bleeding profusely. As the emergency resuscitation was underway, Dr. Chen obtained more details from the patient’s family.
The man had been in a serious traffic accident earlier that day and was initially treated at a nearby hospital. Diagnostic imaging revealed seven comminuted fractures: left distal femur, right tibia, right distal fibula, right calcaneus, right 2nd and 4th metatarsals, and left calcaneus—resulting in massive blood loss and hemorrhagic shock. The local hospital recommended bilateral leg amputation due to the severity of the injuries. However, preoperative testing revealed that the patient had Rh-negative blood, significantly increasing surgical risk and making blood supply difficult. The family then urgently transferred him to Shanghai General Hospital.
“Life is the bottom line, but saving the limbs is hope. No matter how difficult the situation, we must try everything,” said Dr. Zhang Chi, Director of Orthopedic Trauma (North), who immediately authorized an emergency limb-saving surgery. The team’s strategy: stabilize the limbs first, then proceed with reconstructive surgery once the patient was stable.
A Race Against Time: Surgery Through the Night
The hospital activated its highest-level emergency protocol. The Medical Affairs Office (North) and the Department of Transfusion Medicine immediately coordinated with the Hongkou District Blood Bank, which rushed to deliver the first batch of life-saving blood. Under the coordination of anesthesiologist Dr. Zheng Teng and the OR nursing team, the trauma surgeons began operating through the night.
First, they performed thorough debridement on both feet to prevent infection. Then, using Kirschner wires, they temporarily fixed the nearly detached left calcaneus and identified and repaired the ruptured arteries. By 2:10 AM, when the surgical team saw color returning to the previously pale foot, a collective sigh of relief filled the operating room.
Crisis Upon Crisis: Another Emergency, Another Life Saved
The next morning, the patient’s condition deteriorated again. Post-op hemoglobin dropped to a dangerous 48 g/L. The hospital convened an urgent interdepartmental rescue conference, calling on all resources, including district and city blood banks. Dr. Chen, despite working through the night, managed to contact the patient’s Rh-negative siblings in Anhui, who traveled to Shanghai to donate blood.
With support from Dr. Tian Rui (Emergency & Critical Care) and Dr. Li Jinbao (Anesthesiology), the team conducted another emergency procedure: external fixation of the left femur and right tibia/fibula, stabilizing the fractures and minimizing blood loss. The patient’s hemoglobin began to rise, and he gradually recovered from shock.
Fighting Infection, Preparing for Reconstruction
As the patient began to regain consciousness, the team observed increasing drainage from the leg wounds. Lab cultures confirmed Staphylococcus aureus infection. The Clinical Pharmacy Department, led by Dr. Liao Yun, swiftly developed a personalized antibiotic regimen based on susceptibility testing. Meanwhile, the trauma team conducted multiple vacuum-assisted wound closures, gradually controlling the infection.
By June 17, the patient finally met the criteria for definitive reconstruction. Dr. Zhang Chi led the team in performing open reduction and internal fixation (ORIF) for the left femur and right tibia fractures. The surgery was performed with extreme caution; meticulous debridement, anatomical realignment, and precise internal fixation successfully restored two major weight-bearing bones while minimizing intraoperative bleeding—preserving the possibility of future mobility.
Coordinated Recovery: From Wounds to Walking
Postoperatively, Head Nurse Yu Ying led the nursing team in careful wound management. The Rehabilitation Department intervened early with a personalized rehab plan ranging from muscle strengthening to weight-bearing walking. With seamless collaboration among multiple specialties, the patient overcame multiple life-threatening crises. His vital signs stabilized, fractures healed securely, wounds closed well, and on June 24, he was officially discharged.
Source: Wenhui Daily (June 30, 2025)
Reporter: Li Chenyian
Editors: Cai Shishi