- News
Shanghai General Hospital's Professor Li Baiwen's Team Achieves Patient "Rebirth" Through Pioneering Surgical Approach
Recently, the Digestive Endoscopy Department of Shanghai General Hospital (Southern Branch) successfully performed an endoscopic ultrasound-guided gastrojejunostomy (EUS-GE) on a patient with severe pancreatitis complicated by extensive peripancreatic abscesses, intestinal fistula-induced duodenal obstruction, and refractory hyponatremia, establishing a vital "lifesaving pathway" for this critically ill patient.
This successfully performed EUS-GE which is praised to be a dance on the razor's edge not only overcame the limitations of traditional treatments but also pioneered a new chapter in applying EUS-GE technology to complex gastrointestinal obstruction with refractory electrolyte imbalance syndrome caused by severe pancreatitis.
A Desperate Cry for Life
The patient is a 42-year-old male who had developed disconnected pancreatic duct syndrome (DPDS) and extensive walled-off necrosis (WON) in the abdominal cavity following acute severe necrotizing pancreatitis 11 months prior. Despite multiple endoscopic and surgical debridement procedures to control infection, the patient fell into a "vicious cycle" due to pancreatic head abscesses and extensive edema/adhesions from intestinal fistulas, resulting in severe duodenal strictures.
For over a year, the patient could not eat normally, experienced recurrent vomiting of large amounts of gastric fluid, required long-term jejunal feeding tubes and gastrointestinal decompression, developed refractory electrolyte imbalances from prolonged gastric decompression, with recurrent severe hyponatremia episodes leading to shock and coma, the patient endured extreme suffering and severely diminished quality of life. With benign obstruction caused by extensive inflammation: traditional duodenal stents were unsuitable, the patient's extreme weakness, extensive abdominal adhesions, and distorted vascular anatomy made surgical intervention prohibitively high-risk, The case had reached what seemed like a "hopeless dead end."
The Breakthrough Moment—Precision Art on the Razor's Edge
Facing this extraordinary challenge, Prof. Li Baiwen's team carefully analyzed the patient's condition and imaging findings. Drawing on their extensive experience with EUS-guided complex interventions and through multidisciplinary team (MDT) discussions involving gastroenterology, surgery, anesthesiology, and ICU specialists, they ultimately decided to attempt the innovative EUS-GE procedure.
EUS-GE is a recently developed innovative technique that adapts the principles of surgical gastrojejunostomy. Using an ultra-minimally invasive approach, it creates a "bridging pathway" between the stomach and jejunum for patients with pyloric/duodenal obstruction (see Figure 1), while avoiding the significant trauma of traditional surgical methods.
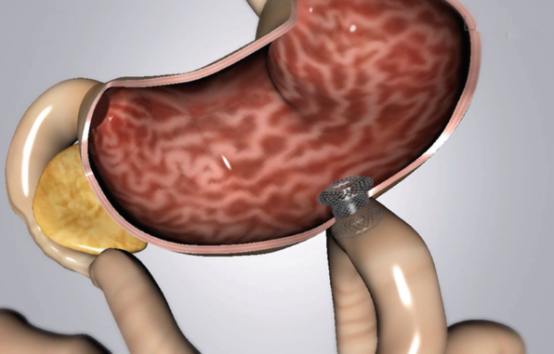
Principle of EUS-GE Procedure
The procedure required precise identification of the target jejunum under endoscopic ultrasound guidance, using a LAMS stent to construct a vital "bridging pathway" between the stomach and jejunum. Every step of the operation demanded meticulous navigation to avoid major abdominal blood vessels and intestinal fistulas, akin to "walking a tightrope."
Prior to surgery, the multidisciplinary team (MDT) meticulously planned for all potential complications. During the procedure, the anesthesiology team provided continuous monitoring. The initial step involved identifying the optimal puncture path under EUS guidance while carefully avoiding blood vessels along the trajectory. Moderate injection of saline and contrast agent confirmed the position of the target jejunum.
The patient's extensive abdominal adhesions resulted in an unusually large distance between the stomach and jejunum, coupled with rapid jejunal peristalsis that created extreme instability. The slightest error could have led to procedure failure and serious complications like intestinal leakage, creating an atmosphere of intense tension in the operating room.
Director Li Baiwen steadily manipulated the puncture instruments, adjusting the approach to synchronize with the jejunum's contraction-relaxation rhythm. At the precise moment of complete jejunal relaxation, he executed a rapid yet technically perfect puncture, securely entering the target jejunal lumen. Under combined EUS and fluoroscopic guidance, the LAMS stent was deployed swiftly.
The entire procedure was completed seamlessly in just five minutes, perfectly establishing the "lifesaving pathway." The deployed LAMS stent bloomed like a beautiful flower between the patient's stomach and jejunum (see Figure 2). Immediate contrast imaging showed rapid passage of contrast agent through the anastomotic channel into the jejunum, immediately relieving the obstruction that had plagued the patient for nearly a year. By the following day, the gastrointestinal decompression tube could be removed, significantly alleviating the patient's suffering.
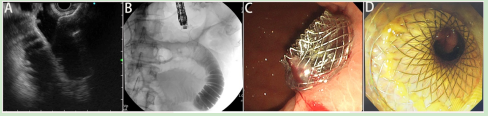
EUS-GE Procedure: (A) EUS-guided transgastric jejunal puncture, (B) LAMS stent anastomosis creation ,(C,D) Successful gastrojejunal anastomosis establishment
Technological Innovation - A New Paradigm in the Minimally Invasive Era
While EUS-GE is typically employed for palliative treatment in patients with advanced malignant obstructions, Professor Li Baiwen's "Huating" endoscopy team—one of China's pioneering centers in this technique—has successfully adapted this innovative approach to address benign, refractory duodenal obstruction caused by severe pancreatitis. This groundbreaking application resolved a year-long complex obstruction, demonstrating remarkable clinical ingenuity. Key Challenges Overcome:Extensive post-debridement abdominal adhesions. Tortuous and complex abdominal vasculature. Disrupted gastojejunal anatomy with long bridging distance. Exceptionally high technical difficulty. Outcomes: Oral intake resumed on postoperative day 1. Dramatic improvement in nutritional status. Transformative enhancement in quality of life.
Epilogue
The Digestive Disease Clinical Medical Center at Shanghai General Hospital (Southern Branch), under Professor Li Baiwen's leadership, has long specialized in endoscopic debridement and drainage for severe necrotizing pancreatitis with peripancreatic abscesses, developing multiple patented innovations and earning provincial-level awards.
This case—from "no way out" to "miraculous recovery"—epitomizes how Professor Li's team: Marries technological innovation with compassionate care. Harnesses precision minimally invasive techniques to restore life. Establishes a new framework for managing complex pancreatitis complications and gastrointestinal obstructions. This textbook-caliber rescue not only opens new therapeutic avenues but also vividly illustrates the boundless potential of interventional endoscopy.
Expert Profile

Prof. Li Baiwen
Deputy Director, Digestive Diseases Clinical Medical Center, Shanghai General Hospital
Executive Deputy Director, Digestive Diseases Clinical Medical Center
Director , Department of Digestive Endoscopy
Academic Credentials
MD, Chief Physician, Doctoral Supervisor
Visiting Scholar, Emory University, USA
Professional Leadership
Committee Member, Shanghai Society of Digestive Endoscopy
Vice Chair, EUS Group, Shanghai Society of Digestive Endoscopy
Committee Member, ERCP Group, Shanghai Society of Digestive Endoscopy
International Committee Member, Japanese Gastroenterological Association (JGA)
Council Member, World Chinese Endoscopist Association
Standing Director of the China Interventional Medicine Non-Vascular
Channel Interventional Innovation Alliance
Peer Review Roles
Editorial Reviewer for:
Gastrointestinal Endoscopy (GIE)
Frontiers in Oncology
Cell Death & Disease
Journal of Digestive Diseases
Awards & Honors
Excellence Award, National EUS Interventional Video Competition
Second Prize, Shanghai Medical Science & Technology Progress Award
Second Prize, Hua Xia Medical Science Progress Award
Shanghai "Outstanding Inventor" Award for Employee Innovation
Shanghai "Pujiang Talent Program" Grant Recipient
Clinical Expertise
Pioneering minimally invasive endoscopic interventions including:
Advanced therapeutic ERCP & EUS
ESD/EVL/POEM/G-POEM procedures
Innovative EUS-ERCP hybrid techniques for complex pancreatobiliary diseases:
✓ EUS-guided biliary drainage (EUS-BD)
✓ EUS-guided pancreatic duct drainage (EUS-PD)
✓ EUS-guided transluminal anastomosis (EUS-TASR)
✓ EUS-NOTES procedures
✓ EUS-directed debridement of pancreatic necrosis
Research Impact
Principal Investigator for 11 competitive grants (NSFC, Shanghai STCSM, etc.)
80+ publications in Gastroenterology, AJG, Endoscopy, etc. (50+ SCI-indexed)
Author/co-author of 10 medical monographs
Holder of 9 medical technology patents (3 commercialized)
Contributor to 5 national clinical guidelines
Outpatient Schedule
Specialty Clinic: Monday & Wednesday mornings