- News
The Department of Endocrinology, Pancreatic Surgery and Other Disciplines of Shanghai General Hospital Cooperated to Complete the Resection of An Insulinoma
In recent months, Mrs. Zhang, a 75-year-old lady had repeated symptoms of cold sweat, hand trembling, dizziness, and even coma at night for many times, and was told that she was suffering from hypoglycemia. The endocrinology department, pancreatic surgery department, radiology department, ultrasound medicine department and other multidisciplinary cooperation of our hospital, after meticulous examination, finally pinpointed and removed the "culprit" that caused Zhang's repeated coma - an insulinoma located in the tail of the pancreas.
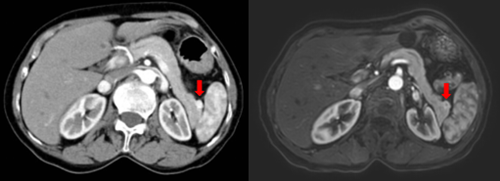
CT dynamic enhancement (left) and magnetic resonance enhancement (right) images of the patient's pancreas, showing a small protruding and enhancing tumor in the tail of the pancreas
Since 2 years ago, Mrs. Zhang has been suffering from panic attacks, hunger and weakness, and many times she went to outside hospitals for examination, but the cause of her hypoglycemic attacks could not be determined. In recent months, Mrs. Zhang's hypoglycemia symptoms have worsened and she has been in a coma at night for several times. Following the suggestion of her family, Mrs. Zhang came to the expert clinic of Professor Liu Fang, the executive director of the Department of Endocrinology and Metabolism of Songjiang Hospital for help.
During her hospitalization, Mrs. Zhang still had early morning hypoglycemia occurring, with the lowest blood glucose of only 1.8 mmol/l. Meanwhile, it was found that the insulin release index (IRI) reached 1.08 (normal below 0.3), and her thyroid function, corticosteroid and GH were normal during hypoglycemia. According to the history and the examination results, insulinoma is the most likely etiology, but it posed some difficulties for localizing the insulinoma. Local diagnosis is the key to confirm the diagnosis and surgical treatment of pancreatic islet b-cell tumor. However, insulinoma is often extremely small in size, and its localization and diagnosis is a clinical difficulty.
The medical team first performed an enhanced MRI of the pancreas, but the first review did not find clear signs of insulinoma, so the patient was further arranged to receive an enhanced CT examination of the pancreas. At the same time, a multidisciplinary collaboration was organized, inviting Long Jiang, director of the Department of Pancreatic Surgery, Dr. Wang Zhongling, chief physician of the Department of Radiology, Dr. Du Lianfang, chief physician of the Department of Ultrasound Medicine, and Shi Qiusheng, executive director of the Department of Ultrasound Medicine in the south. After performing pancreatic ultrasonography and repeatedly reading and discussing her pancreatic MRI and CT-enhanced imaging data, the expert team finally found an adenoma of less than 2 cm in the tail of the pancreas.

After the diagnosis was confirmed, Mrs. Zhang was transferred to the pancreatic surgery department to undergo insulinoma resection. What was seen intraoperatively was consistent with the preoperative imaging judgment, and a mass of about 2 cm was found in the tail of the pancreas. Under the guidance of Long Jiang, the caudal pancreatic tumor was resected with preservation of the spleen using laparoscopic combined with intraoperative ultrasound guidance and precise localization. The patient recovered and was discharged 7 days after surgery without further hypoglycemia.
During this consultation and treatment, medical and nursing staff practiced the hospital's "patient-centered" concept with their excellent diagnosis and treatment, highly responsible spirit, warm medical service and efficient treatment mode. It also fully demonstrated the advantages of multidisciplinary cooperation and the comprehensive strength of Shanghai General Hospital.
(Correspondent/Fan Nengguang, Southern Endocrinology Department)